
In this August issue we launch our vaccination schedule webpage, attend and present at conferences including VH2025, deep dive into community video co-design, collaborate with Justice Health and much more…
- Hepatitis A and B Vaccine Schedule for Adults
- Culture is not a Barrier, it is the Key to Connection
- Viral Hepatitis Conference 2025
- HEP CURED Hepatitis Awareness Week: Hepatitis NSW collaborates with Justice Health NSW
- Healthcare in Secure Settings Conference 2025
- Key hepatitis related observations from attending Healthcare in Secure Settings Conference 2025
- Colette McGrath’s retirement farewell
Hepatitis A and B Vaccine Schedule for Adults

People at risk for hepatitis A or B can get tested and vaccinated to protect their liver health. We’ve developed a webpage covering the details.
Go to Hepatitis A and B vaccine schedule for adults for more information, and download the vaccine schedule here
Getting your hepatitis A and B vaccinations is an important step in protecting yourself and others.
The hepatitis A and B viruses can cause liver infections that can lead to serious illness. The good news is, you can be vaccinated against both hepatitis A and B! The vaccinations are safe and effective.
Hepatitis A vaccine
The hepatitis A vaccine is especially recommended if you are:
- travelling to a country where hepatitis A is common
- living with a liver disease or hepatitis B or C
- a man who has sex with other men (MSM)
- a person who injects drugs
- a person whose occupation is at higher risk for hepatitis A, such as childcare, health care, plumbing, sewerage work.
- Aboriginal and Torres Strait Islander children in some areas.
Go to Hepatitis A and B vaccine schedule for adults for more information.
Hepatitis B vaccine
If you are at risk for hepatitis B, you can get a hepatitis B test. If you test negative, you can get the hepatitis B vaccine. If you test positive you can live a long and healthy life by having regular monitoring and taking medication if needed.
Hepatitis B can only be passed on through blood-to-blood contact, unprotected sex or during birth.
Go to Hepatitis A and B vaccine schedule for adults for more information.

Culture is not a Barrier, it is the Key to Connection
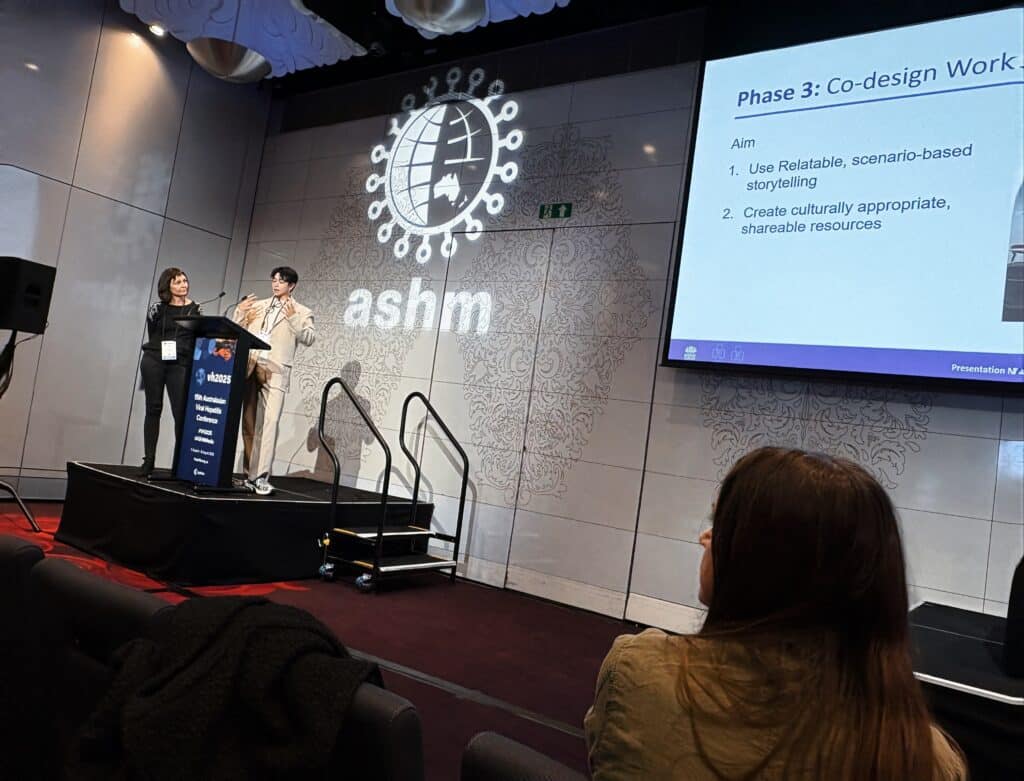
Regular readers of The Champion will recall last month’s story about our Hepatitis B and Multicultural Team co-designing Mandarin videos and posters about living with hepatitis B. Below is an expanded description of that design process presented at the Australasian Viral Hepatitis Conference VH2025 by Willis, Project Officer, Hepatitis B and Multicultural Liver Health with Hepatitis NSW, and Sarah (Sexual Health and Blood Borne Virus Services, South Eastern Sydney Local Health District).
One of the presentation’s key messages coined by Willis was “Culture is not a barrier, it is the key to connection.” This phrase was selected as the most memorable sentence of the conference during the closing ceremony.
“We began in early 2023 by forming a multidisciplinary working group of bilingual staff from health services, community organisations, clinicians, and researchers. Our shared aim was to improve hepatitis B knowledge, reduce stigma, and strengthen care pathways through a culturally appropriate campaign. Our strategy was to consult widely, co-design resonant materials, develop content in-language (not mere translations), and map clear referral pathways.
- Phase 1 build trust and set the tone.
- Phase 2 — an online survey (200+ responses) and four in-depth consultations (34 participants) — revealed strong demand for clear information on transmission, testing, and treatment, and a preference for real, visual stories. Knowledge increased by 30% after sessions.
- Phase 3 used scenario-based storytelling to capture everyday moments of stigma, turning them into four short videos and four posters. Ten community members shaped every detail in workshops, from colours to slogans.
- Phase 4 focuses on dissemination and evaluation: a soft launch during Hepatitis Awareness Week 2025, rollout via GPs, community organisations, and trusted (WeChat, YouTube, RED, WhatsApp, Facebook), with analytics and feedback guiding refinement.
Key Messages:
Co-Design is Essential: Co-design must guide the process, from the start to the end. Communities should be engaged as equal partners. Not just consulted but genuinely heard. Their experiences and voices shaped every aspect of the content.
Prioritise Cultural Relevance: Use familiar languages, imagery, and platforms that resonate with the community. Resources should be created in-language from the outset—not simply translated from English word to word. No google translate! Share them through trusted, culturally relevant channels to ensure they truly reach and reflect the audience. When resources align with how people naturally communicate and understand health, trust is built, and it encourages actions.
Focus on Stigma: Stigma is not just misinformation, it is people being pushed to the margins, isolated, excluded, and made to feel less than. Stigma hurts. And we have the power, and the responsibility, to change that. We need to go beyond clinical facts, to create space for open, honest, human conversations.”
You can find the poster here

Viral Hepatitis Conference 2025

In August Hepatitis NSW headed down to Naarm/ Melbourne for the Australasian Viral Hepatitis Conference (VH25). A welcome staple in the calendar, this year’s conference had big shoes to fill after last year’s excellent conference in Darwin. The conference took a novel approach by handing the reins to affected communities to drive the agenda and it paid off with a wonderful shift in focus. Highlights included renewed focus on hepatitis B, and a possible future point-of-care ALT test, lots of usable new data, some great work on stigma reduction, and much more!
Pip was proud to present the work of the EMPOWER Program over the last 2 years but, more than that, she was totally in awe of the shared energy and passion of the conference; a sentiment shared by the team as we took inspiration from themes like integration, co-design, and implementation. It was great to see so much emphasis on peers and their crucial contribution to eliminating hepatitis C in partnership with amazing healthcare teams and researchers. The conference was also an opportunity to catch up with friends and program partners who we rarely see in person. The range of speakers and sessions on offer showed the diversity in the sector, including the variety of work and projects being delivered to viral hepatitis affected communities around Australia.
In addition to our EMPOWER presentation Hepatitis NSW engaged in spotlight sessions, with five-minute presentations with Q&A at five tables. Liam presented our lived experience peer worker program which celebrated the significant milestone of 20K+ engagements and the continued importance of lived experience practitioners working across the organisation and out in the community. Session participants were highly engaged, with a range of sector representatives asking questions about Hepatitis NSW’s lived experience peer worker programs and the work and approaches it took to achieve the different program successes.
Mina presented a tabletop presentation “Write to Be Heard – Hepatitis B Stories from the Chinese and Korean Communities”. This tri-lingual book – available in ENGLISH, CHINESE and KOREAN– contains personal stories detailing lived experience from people in NSW communities affected by hepatitis B. It was developed following a writing competition and the winning stories were published. It is one part of Hepatitis NSW’s ongoing work in community engagement around hepatitis B and efforts to increase knowledge and testing and reduce stigma. ‘Write to Be Heard’ can be posted out. Email mkim@hep.org.au with your address, language and quantity.
And finally, a conference would not be a conference without the posters. Oral poster presentations have been a great component of ASHM’s Viral Hepatitis Conference programs, giving abstract authors who did not receive a concurrent session a spot to present on their work to delegates, and receive questions and feedback during designated tour sessions.
Grace and Maia spoke to their poster which summarised the wealth of findings from Hepatitis NSW’s consultations with First Nations people across the state on motivators and barriers to hep C testing and treatment. The project was completed in partnership with members of the HIV/Hepatitis and Related Programs (HARP) Aboriginal Health Workers Network (HAHN) who contributed logistics and promotion/organisation of both face-to-face community consults, interviews, and development and distribution of the online survey.
We sought information on people’s understanding of exposure risk, actual exposure risk, and previous exposure to hepatitis C along with cure and/or awareness of cure. There was also a link to our state-wide awareness campaign – HEP CURED – in which the suitability, or otherwise, of the existing imagery and messaging was gauged. Outcomes from the project led to the establishment of a HEP CURED First Nations Reference Group and recommendations on developing a culturally appropriate hep C campaign.
Hepatitis C testing and treatment motivations for First Nations communities >>
Yarnin’ About Hep B in Custody: Supporting Our Mob Inside >>
Click on the link below to see all of Hepatitis NSW’s poster submissions.
https://www.hep.org.au/resources/poster-presentations/

HEP CURED Hepatitis Awareness Week: Hepatitis NSW collaborates with Justice Health NSW
This month, the Harm Reduction team from Justice Health NSW were joined by Hepatitis NSW staff for a Hepatitis Awareness Week event held at South Coast Corrections in Nowra. Allan – Senior Aboriginal Harm Education and Sexual Health Officer, who was profiled in last month’s Champion for his work co-designing hepatitis prevention strategies with Aboriginal people in custody, led the event with Gary, the Manager of Harm Reduction Projects.
A lively patient education event was set up to engage inmates with conversations on hepatitis C prevention. The highlight was the interactive quiz on using Fincol to disinfect personal items – sparking plenty of real-world conversations. More than 80 patients took part, walking away with prizes – beanies, water bottles, and the ever-popular cappuccino sachets. The day was supported by the Public Health nurses, who ran an open clinic alongside and saw over 20 patients for hepatitis C testing, blood pressure checks, and other primary care needs. These events take months of preparation and there is appreciation for the support of those who make these events possible – with mentions to Governor Lennox Peter, and the nursing team.

Healthcare in Secure Settings Conference 2025
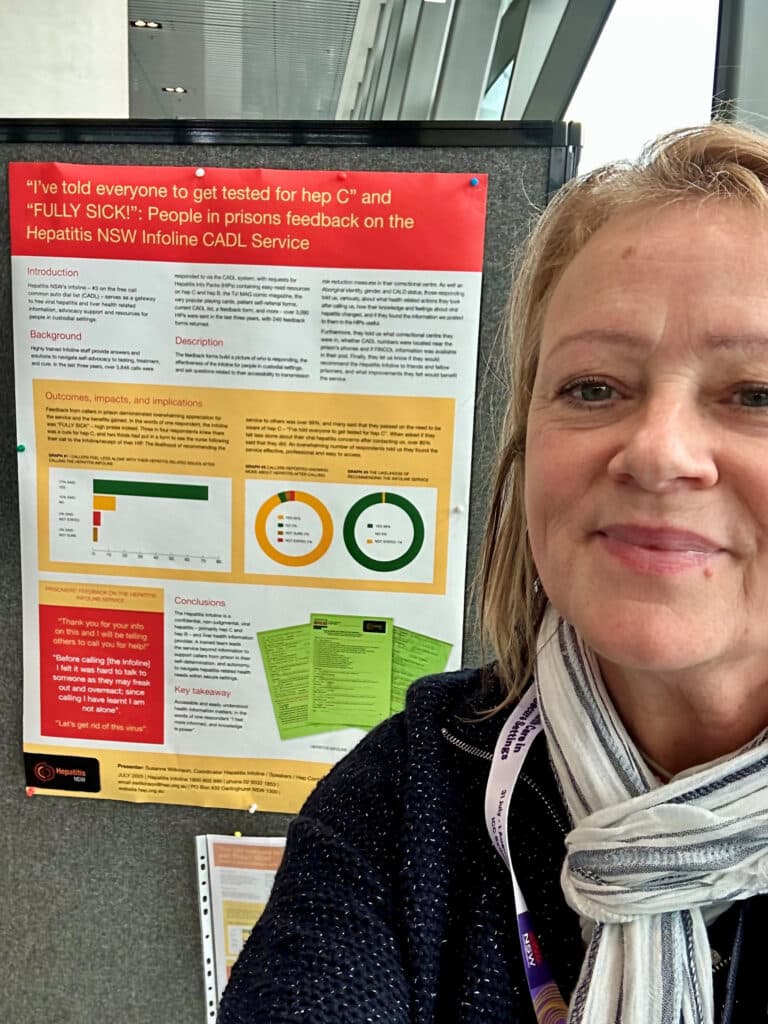
Hepatitis NSW was represented by Susanne at Justice Health’s Healthcare in Secure Settings Conference 2025, with a poster titled “Fully Sick”. (Fully sick is Australian slang for cool or great.) The poster highlighted the overwhelmingly positive feedback received from people in prison, gathered through the feedback form included in our Hepatitis Information Packs (HIPs).
People in NSW prisons can seek hepatitis related information and support by calling the Hepatitis Infoline for free by dialing #3 on the Common Auto Dial List (CADL). They can also request one of our HIPs to be sent to them. Each HIP includes printed hepatitis-related information, a feedback form, and pre-addressed, stamped envelopes for returning the feedback forms. The feedback forms are designed to assess satisfaction with the Infoline service delivery and the usefulness of the printed information provided.
Our “Fully Sick” poster, showcased at the conference, reflects the strong impact of Hepatitis NSW’s efforts to support people in prison through accessible, practical health information and services. The positive feedback we receive highlights the value of the Hepatitis Information Packs and the Infoline service in addressing the needs of people in prison. By continuing to provide trusted resources and a direct line to support and opportunities to have their opinions on the service provision heard, Hepatitis NSW is helping to empower individuals in prison to make more informed decisions around their health.
To view the poster, please click here

Key hepatitis related observations from attending Healthcare in Secure Settings Conference 2025
Our Hepatitis NSW colleague, Susanne (Coordinator – Infoline and Related Programs, Community Support & Engagement) recently attended Justice Health’s Healthcare in Secure Settings Conference 2025. The following report is Susanne’s hepatitis-related observations over the two days.
Supporting individualised care and health equity for people in prison and
returning to the community
Justice Health reported throughout the conference that, as their efforts to improve the health and well-being for people in prison continues to gain momentum, it’s critical to address the complex, intersectional needs that shape their healthcare experiences — both inside prison and upon return to the community. This includes ensuring that opioid treatment support, hepatitis related care, and health literacy initiatives are accessible, person-centred, and respectful of individual choice.
Opioid treatment on return to community should be a choice — not an assumption
Opioid Treatment Programs (OTPs) are often offered as part of the transitional care for people re-entering the community after incarceration. While these programs can be lifesaving for many, it’s important to recognise that they are not suitable for everyone. Mandating or heavily promoting OTP as a default without considering individual needs, histories, and preferences risks undermining autonomy and engagement.
A person-centred approach to opioid substitution therapy (OST) acknowledges that treatment success depends on readiness, informed consent, and access to a range of options. People leaving prison should be supported to make informed decisions about their care, rather than being steered into pre-determined pathways. This includes providing transparent information, respecting those who wish to explore abstinence-based options, and ensuring access to broader supports such as linkage to care and other services according to their hierarchy of needs.
Intersectional needs in hepatitis care: Going beyond a single diagnosis
Hepatitis B and hepatitis C remain disproportionately prevalent in prison populations, particularly among people who inject drugs. Yet effective hepatitis care requires more than a narrow focus on viral treatment. A holistic, intersectional approach must account for the layered challenges individuals face — including substance use, mental health issues, trauma histories, and chronic physical conditions.
Addressing hepatitis in prisons and post-release settings means ensuring that OST is offered and on uptake well-integrated into care plans, that mental health support is readily available, and that screening and treatment for hepatitis are delivered in non-stigmatising, non-discriminative and culturally safe ways. Many people in custody come from communities that experience systemic disadvantage, including Aboriginal and Torres Strait Islander peoples, people with disabilities, and those with histories of poverty and homelessness. Care must reflect this reality.
By recognising the interplay of these factors, health services can better support individuals through hepatitis screening, linkage to care, and treatment adherence — ultimately improving better health outcomes and reducing community transmission.
Increasing health literacy behind bars
Improving health outcomes in prison also requires a focus on health literacy — the ability to find, understand, and use information to make informed decisions about personal health. Many people entering custody have had limited access to quality healthcare and education and may not feel empowered to ask questions or advocate for themselves.
Tailored, linguistically diverse and culturally appropriate health education can make a significant difference. This includes explaining medical processes in plain language, using peer educators, and offering resources that address and how to navigate the unique challenges of prison life. Boosting health literacy equips people with the knowledge they need to understand diagnoses, consent to treatment, and navigate healthcare systems both within the prisons and upon release.
Importantly, enhancing health literacy is not just about individual empowerment — it’s a matter of public health. As individuals move between prison and community settings, the ripple effects of increased knowledge and confidence can support healthier families, reduced disease transmission, and more effective use of health services.
Conclusion
Supporting people in prison, and those returning to the community, requires flexible, trauma-informed, and person-centred approaches. This means offering choices in treatment options like OTP, addressing intersecting needs in hepatitis care, and improving health literacy across the board. When we centre the voices and experiences of those affected, we create more just and effective systems that support long-term health outcomes and dignity for all.

Colette McGrath’s retirement farewell

Colette with Carolyn Murray (Director of Population Health), Douglas (former SES LHD HARP Health Promotion), Tracey (Justice Health), Wendy (KRC) and Dr Ingrid van Beek (former Director of KRC and MSIC).
Colette McGrath is a highly respected health professional and has been described by others in the sector as “the giant on whose shoulders we stand”. With her recent retirement she leaves a legacy in hepatitis C elimination and health equity. Hepatitis NSW went along to Colette’s retirement event and learnt about her work.
Colette has dedicated her career to nursing, harm minimisation, and blood-borne virus (BBV) work, arriving from Northern Ireland in the 1980s to work in North London. At the time, hepatitis C was still known as “Non-A Non-B hepatitis,” and little was understood about its transmission. Colette witnessed firsthand the stigma and discrimination faced by people who injected drugs, gay men, and haemophiliacs, which deeply influenced her commitment to compassionate care.
After migrating to Australia in 1994, Colette joined the Kirketon Road Centre (KRC), later becoming Clinical Services Manager at the Medically Supervised Injecting Centre (MSIC), and working with the HARP Unit in South Eastern Sydney Local Health District. She collaborated with key organisations including Hepatitis NSW, NUAA, ACON, Positive Life, and BGF, helping to shape services that were accessible and stigma-free.
Colette was a pioneer in integrating peer workers and community development into clinical models, ensuring marginalised populations received care in environments they could trust. Her leadership helped transform outreach and clinical services into inclusive, community-driven models.
In 2016, Colette turned her focus to hepatitis C elimination efforts in NSW correctional facilities. At Justice Health, she led efforts to ensure testing and treatment continuity for incarcerated individuals, even as they moved between prisons. Her work was instrumental in adapting services to new treatment options and models of care.
Colette led the implementation of the micro elimination model of testing and treating people in custody, creating communities of people who had been tested and cured in the wings or pods, or entire correctional centres that were, in effect, hep C free.
Enjoy retirement!

The Champion is our free monthly eNews with updates on hep C, hep B, treatment news, social media campaigns, living well with viral hepatitis, and events. To subscribe and receive a monthly edition of the The Champion to your inbox, please complete this confidential form:







